
I brought it in to my school science class, of course, and showed it around. After a while, my parents got nervous about having it in the house, even though it was in a jar that was inside another jar. So how do you get rid of an insect you don't want? We used the usual high-tech method. We took it outside, dropped it out onto the concrete, and stepped on it. But in general, the outdoor creatures of my childhood were pretty benign. Things seem to have gotten much worse since then. Where we live in eastern Massachusetts, mosquitoes can carry Eastern Equine Encephalitis, which is frequently fatal. And deer ticks, which are all over the place, carry Lyme disease, which can cause serious problems if you don't catch it early. We have a nice back yard, but are leery of spending too much time there in the Summer and Fall. Margie and I have both had early Lyme disease, and were both successfully treated with antibiotics. We routinely check our bodies for deer ticks if we've been outside. These tiny ticks are much smaller than dog ticks, and hence much harder to spot. We used to have a doctor, separate from our regular internist, whom we called our "Travel Doctor". He was Leonard Marcus, and we always consulted with him before any trips taken by us or by our daughters (who did a lot more third-world travel than we did). An infectious disease specialist, he also was a parasitologist, and we brought him any ticks that we pulled off our bodies (that is, assuming they were actually attached and biting, and not just walking around). Dr. Marcus would put them under his microscope, identify the species and stage, whether or not it was engorged with blood, and tell us what action needed to be taken.
The reason Dr. Marcus had gotten so excited is that I was the first person to ever bring him a larval deer tick - they are so tiny, almost nobody manages to spot them. Most of the ticks people bring him are nymphs or adults.
The rash can also be atypical. Margie was once bitten between two toes, and it was hard to discern the circular nature of the rash (and to make a differential diagnosis between Lyme disease and cellulitis, which can be more quickly dangerous). But in the end Lyme disease was the conclusion, and it responded quickly to a short course of doxicycline. It was Margie who was victimized by our oddest parasite. She never stinted on her regular mammograms, having had breast cancer at a fairly young age (described in my earlier entry Remembrance of things breast). By the way, we discovered you do get a discount on your mammogram if you have only one breast. In any event, in 1993, one of these mammograms turned up something odd. It looked more like a cyst than a solid tumor, and it was followed up with a more detailed mammogram and a sonogram, equally inconclusive. Well, when you've had a previous cancer, you don't mess around with these things, so it was quickly biopsied. And then we waited and waited for the results, a rather anxiety-producing process. What was taking so long? It ultimately turned out that the biopsy slides were being passed around to a few doctors for an opinion. When we finally got the report, it read "Granulomatous response to necrotic cestode larva consistent with cysticercosis."
Cysticercosis is a condition that results when a human, instead of a pig, ingests fecally contaminated food containing the tapeworm's eggs. As in the pig, these hatch, and move into the tissues of the host. But a human being, not the normal target of these larvae, is better able to fight them off. The body attacks the larvae, forming cysts around them, and eventually kills them off. The diagnosis made sense of some symptoms Margie had had earlier, as she had detected two previous hard cysts on her body, of unexplained origin. But these had not seemed worthy of further study, and were passed off as insect bites or some other form of minor irritation. Now they made sense - they were cysticercosis cysts. But only when one had appeared in the breast (an unusual location for them) had it warranted biopsy. One further complication. While the breast is an unusual location for a cysticercosis cyst, the brain is not - the larvae go there in about sixty percent of the cases. And an MRI revealed that they had done so in Margie's case. She had three Rice Krispies-sized larvae in her brain. When she asked the doctor what they were eating, he replied, "You don't want to know". But cysts in the brain can produce convulsions, which of course can be quite dangerous (especially if you're driving at the time). Treatment is not required - the larvae will eventually die off on their own. But it's generally thought better to kill them off in a controlled environment, while watching for the possibility of seizures. Margie was put on Dilantin, an anti-convulsive drug, while awaiting treatment with an anti-parasitic agent, albendazole. She was then treated in-patient at Massachusetts General Hospital, on a seizure watch,Note 2 while on both Dilantin and steroids. When multiple larvae are killed at once, the result can be a seizure-producing inflammation. She stayed on the Dilantin for about a year after the treatment, as an anti seizure precaution, with rather nasty side-effects. She was eventually weaned off it, after another MRI showed the larvae in the brain to be completely gone.Note 3 We never determined where Margie picked up the cysticercosis in the first place. When it was diagnosed, the first question was, "Where have you been traveling?", as it is rarely contracted within the United States. Our most likely candidate was Mexico, or possibly Jamaica, although the timeframe seemed off for the latter. It was a rather unpleasant episode. The only benefit was that for some time afterwards, Margie was rather well known in the Mass General Mammography center. Whenever she mentioned the episode when coming in for a mammogram, the staff would smile at her, saying, "Oh - you're the woman whose cysticercosis we found on a mammogram - pleased to meet you!" She was famous.
For instance, if I eat raw tuna from a reputable sushi restaurant once a week, what is the probability that I'll have one or more problems with a parasite over a thirty year period? Is it miniscule? Or greater than fifty percent? I haven't got the faintest idea. Based on a short letter by nutritionist Jean Mayer in the Boston Globe, we do favor raw tuna, and seldom eat raw salmon. Because salmon spend a portion of their life cycle in fresh water, they are apparently more prone to parasites than fish like tuna which are purely salt-water dwellers. Margie did once ask our above-mentioned travel doctor, Leonard Marcus, about sushi. He replied ominously, "I love sushi. I don't eat it myself, but [because of sushi] I get to see a lot of interesting worms."
  Note 1: Dr. Marcus explained the life cycle of the tick to me. After hatching from an egg, a tick passes through three stages in its life, and needs to eat one blood meal in each of these in order to advance to the next stage. The stages are larva, nymph, and adult. It can pick up the spirochete that causes Lyme Disease, Borrelia burgdorferi, by biting an infected person, or, more likely, an infected deer or mouse. It can then pass the disease on when it bites again in its next stage. A larva has had no previous opportunity to pick up the disease - transfer of the spirochete via the eggs has never been documented. [return to text] Note 2: Mass General is, in general (no pun intended) an excellent hospital, but I was not impressed by their "seizure watch". Margie was just confined to her room, at great expense, but was not monitored in any way that I could detect. People didn't even drop into the room on a regular basis. [return to text] Note 3: Maintaining a desired level of Dilantin requires adjusting the dosage based on the serum level determined by frequent blood tests. The infectious disease specialist treating Margie seemed to be so concerned about seizures that she kept Margie's serum level of Dilantin on the high side of the therapeutic range. When we had her consult with a doctor more familiar with the drug, we were told that since the high serum level was producing uncomfortable side-effects, the dosage could be lowered without any loss of seizure protection. Always the Engineer, I created an Excel spreadsheet to track Margie's Dilantin serum level. Once I had three data points, I could calculate the half-life of the drug in the bloodstream, and predict what Margie's serum concentration would be on each blood test. For a while, my calculated predictions were extremely close to the measured values. The only problem was that the half-life I obtained was quite different from the half-life listed for Dilantin in the Physicians' Desk Reference ("PDR"). And then suddenly on one blood test, the value obtained was way off my calculation. Something had changed. I found out that when faced with high Dilantin levels, the body starts generating new enzymes for metabolizing it, and the half life of the drug in the body changes considerably. It is the half-life for long-term treatment that's listed in the
PDR. [return to text]
 |
 Bedbugs like the one shown to the left have been much in the news lately, with major epidemics having been reported in 2010. Since we travel reasonably often, and they are often picked up in hotel rooms, we're following these reports closely, but we've never encountered them.
Bedbugs like the one shown to the left have been much in the news lately, with major epidemics having been reported in 2010. Since we travel reasonably often, and they are often picked up in hotel rooms, we're following these reports closely, but we've never encountered them.
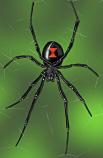 During my childhood in Great Neck, New York, on Long Island just east of New York City, we used to play outdoors with nothing to fear. I did find a black widow spider once. I noticed the classic red hourglass mark on its underside, which I saw after turning it over with a stick (see the photo to the right). As a science oriented kid with a father trained in biology, I had no trouble identifying it.
During my childhood in Great Neck, New York, on Long Island just east of New York City, we used to play outdoors with nothing to fear. I did find a black widow spider once. I noticed the classic red hourglass mark on its underside, which I saw after turning it over with a stick (see the photo to the right). As a science oriented kid with a father trained in biology, I had no trouble identifying it.
 On one occasion, I brought him a tick that looked like the one to the left. That's not the actual size - it was the size of a pinhead. When Dr. Marcus looked at it, he got very excited. "Take a look", he said, motioning me over to the microscope. "Count the legs", he added. I clearly saw six legs. Dr. Marcus told me that meant it was a first-stage tick, a larva, and not a nymph or an adult. It also meant I had nothing to worry about.
On one occasion, I brought him a tick that looked like the one to the left. That's not the actual size - it was the size of a pinhead. When Dr. Marcus looked at it, he got very excited. "Take a look", he said, motioning me over to the microscope. "Count the legs", he added. I clearly saw six legs. Dr. Marcus told me that meant it was a first-stage tick, a larva, and not a nymph or an adult. It also meant I had nothing to worry about.  Unfortunately, Dr. Marcus has now retired, and I know of no other doctor in the Boston area who can provide the information about ticks that he did. If you can treat a potential Lyme infection before the rash develops, the required antibiotic treatment is very short. But now, doctors just advise watching the site of a deer tick bite to see if the bull's-eye rash characteristic of early Lyme disease develops. This is really not adequate advice, as a rash doesn't always show. If it turns out that you are infected, but no rash comes up, you will not be treated early, and could be in for a long and possibly even debilitating bout with the disease.
Unfortunately, Dr. Marcus has now retired, and I know of no other doctor in the Boston area who can provide the information about ticks that he did. If you can treat a potential Lyme infection before the rash develops, the required antibiotic treatment is very short. But now, doctors just advise watching the site of a deer tick bite to see if the bull's-eye rash characteristic of early Lyme disease develops. This is really not adequate advice, as a rash doesn't always show. If it turns out that you are infected, but no rash comes up, you will not be treated early, and could be in for a long and possibly even debilitating bout with the disease.
 What the heck was that? A pork tapeworm called Taenia solium (T. solium, left) normally lives in the digestive tract of humans, casting off eggs. These are ingested when a pig eats fecally contaminated food. The eggs hatch, and the larvae bore into the flesh of the pig. When a human being eats inadequately cooked meat of the pig, the larvae mature into tapeworms, and the cycle is completed.
What the heck was that? A pork tapeworm called Taenia solium (T. solium, left) normally lives in the digestive tract of humans, casting off eggs. These are ingested when a pig eats fecally contaminated food. The eggs hatch, and the larvae bore into the flesh of the pig. When a human being eats inadequately cooked meat of the pig, the larvae mature into tapeworms, and the cycle is completed.
 There's one more parasite question I'd love to have answered. I've never found an answer anywhere, not even on the internet (not even a bad answer). We eat a lot of sushi, which contains raw fish. Just what is the parasitic risk of this?
There's one more parasite question I'd love to have answered. I've never found an answer anywhere, not even on the internet (not even a bad answer). We eat a lot of sushi, which contains raw fish. Just what is the parasitic risk of this?